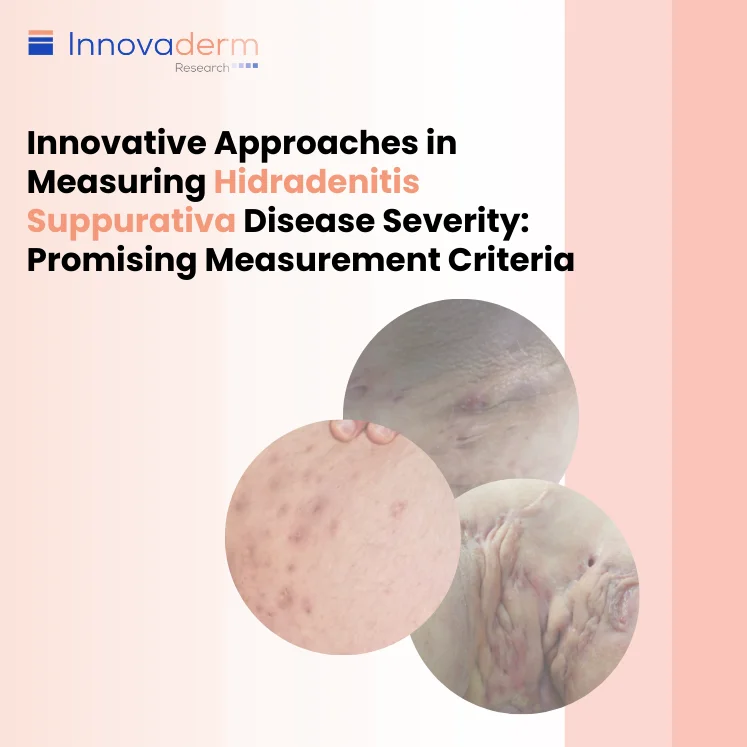
 The challenge of assessing hidradenitis suppurativa (HS), primarily resides with the raters rather than the measurement instruments. In an attempt to find potential solutions to high inter-rater variability in disease assessment, this article will examine the most frequently evaluated endpoints in HS trials, the Hidradenitis Suppurativa Clinical Response (HiSCR), and 2 emerging measures, the International Hidradenitis Suppurativa Severity Score System (IHS4) and the Hidradenitis Suppurativa Investigator Global Assessment (HS-IGA).
The challenge of assessing hidradenitis suppurativa (HS), primarily resides with the raters rather than the measurement instruments. In an attempt to find potential solutions to high inter-rater variability in disease assessment, this article will examine the most frequently evaluated endpoints in HS trials, the Hidradenitis Suppurativa Clinical Response (HiSCR), and 2 emerging measures, the International Hidradenitis Suppurativa Severity Score System (IHS4) and the Hidradenitis Suppurativa Investigator Global Assessment (HS-IGA).
Current Endpoint in HS Trials: HiSCR
One of the current endpoints in HS clinical trials, known as HiSCR, entails a meticulous assessment of abscesses and inflammatory nodules (AN) count.
It measures responses on a dichotomous basis where HiSCR50 responders are characterized by a minimum of 50% improvement in the AN count relative to baseline, with the condition that there should be no increase in abscesses and/or draining fistulas count.
An aspect of fistulas that has raised concerns is that, despite their technical inclusion in the assessment, they are not considered in the response. Patients themselves often emphasize the importance of assessing fistulas, which prompts reflection upon their exclusion. There has been some discussion, including comments from the Food and Drug Administration (FDA) regarding the omission of fistulas from the response evaluation; sparking questions regarding the significance of tunnels in the assessment. However, the consensus leans toward maintaining the existing approach, at least for the time being.
Candidate Endpoints in HS Trials: IHS4
IHS4 was initially validated as a continuous scale. However, to align with FDA preferences, it was later revised to a dichotomous scale. This dichotomous response is defined as a 55% reduction in the total IHS4 score compared to baseline. This change provides a more cohesive and streamlined approach to measuring outcomes.
The construct bears striking similarity to HiSCR, with one notable exception—it includes tunnels into the response assessment and assigns them a substantial weight, 4 times that of nodules, potentially due to patients’ assertions of the problematic nature of tunnels.
Total IHS4 score =
Number of nodules x1 +
Number of abscesses x2 +
Number of draining tunnels x4
When a subject experiences a decrease of 55% or more in their IHS4 score from baseline, it is referred as achieving an IHS4-55.
While this adjustment may seem justified, it also brings up the issue of unpredictability. Nevertheless, IHS4-55 has been validated across various psychometric properties, confirming its efficacy as a dichotomous response. A relevant limitation remains—the need for recognizing and distinguishing the 3 principal lesion types; a task that even the most experienced raters often struggle with.
Candidate Endpoint in HS Trials: HS-IGA
Another instrument in the HS assessment toolkit, the HS-IGA offers a distinct approach. The assessment scale ranges from 0 to 5 and is a format that is well regarded by the FDA for dermatological diseases. It stands out for its inclusivity, which makes it a cohesive and comprehensive tool for evaluation. HS-IGA encompasses all 3 primary HS lesions and their variations without requiring distinction.
Whether an abscess is draining or non-draining, or a nodule is inflammatory or not, this instrument mandates their inclusion in the assessment. The advantage is that there is no requirement for differentiation, potentially mitigating one of the key limitations in HS assessment. It parallels other global scales while streamlining lesion recognition.
Due to its simplicity and feasibility, HS-IGA achieved consensus within the Hidradenitis Suppurativa Core Set International Collaboration (HiSTORIC) research group for use in clinical practice.
- HS-IGA is scored as a number between 0 and 5 based on the sum of abscess (A), fistula (F) (draining and non-draining), and nodule (N) (inflammatory and non-inflammatory) counts, either in the upper or the lower body region, whichever is greater.
- Response is defined as a 2-point reduction in HS-IGA score relative to baseline.
Characteristics of Candidate Endpoints
| Measure | Distinction Among Lesions | Maximum lesion counts |
| HiSCR | 3 lesion types: inflammatory nodules, abscesses, draining fistulas | Unlimited |
| IHS4 | 3 lesion types: Inflammatory nodules, abscesses, draining fistulas | Unlimited |
| HS-IGA | None | Up to 21 abscesses, nodules (inflammatory or non-inflammatory), and/or fistulas (draining or non-draining) |
In considering these 3 measures, HiSCR remains the current endpoint of choice, a preference upheld by the FDA despite requests to explore alternatives. Mastering the recognition, distinction, and accurate counting of the 3 main HS lesions remain fundamental aspects in improving HS assessments. The potential solutions offered by IHS4-55 and HS-IGA shine a light on the intricate landscape of HS assessment, inviting reflection on how we can navigate this complex terrain more effectively.