The Role of Skin barrier Dysfunction in Atopic Dermatitis—The Microbiome

Table of contents
- Cutaneous Dysbiosis Interplay
- S. aureus: Its Interaction and Impact on Skin
- S. aureus and Inflammation
Focusing on the microbiome, Staphylococcus aureus (S. aureus) is a widespread bacterium that produces a multilayer biofilm, was shown to colonize the skin and play a critical role in Atopic Dermatitis (AD). Over 70% of people are colonized, and heavy colonization is associated with skin barrier dysfunction, food allergies and unresponsiveness to cyclosporine. A paper published by Heidi Kong et al. shows that before an AD flare, S. aureus outcompetes other microbial communities, becoming the dominant pathogen on the skin surface during a flare. Post-treatment, some diversity of microbiome colonies is restored. S. aureus outcompetes other microbial communities, becoming the dominant pathogen on the skin surface during a flare. Post-treatment, some diversity of microbiome colonies is restored.
1. Cutaneous Dysbiosis Interplay
An abundance of S. aureus can exacerbate skin flare-ups. Heidi Kong’s team studied the question whether AD lesions or cutaneous dysbiosis occurs first. The answer is complex. It has been found that non-staphylococcus bacteria are protective against AD. Thus, individuals with a high colonization of non-staphylococcus tend to have less severe AD, while others may have staphylococcus colonization preceding AD.
2. S. aureus: Its Interaction and Impact on Skin
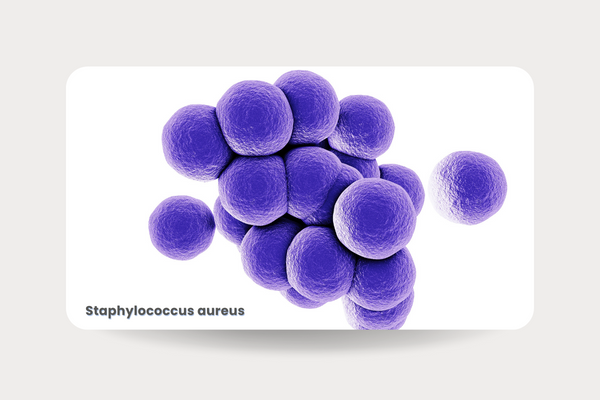
S. aureus is uniquely adapted to human skin as it adheres easily allowing disruption of the skin barrier and drives inflammation. These mechanistic functions make S. aureus difficult to eliminate as it is perfectly designed to latch onto skin and corneal surfaces. Under atomic microscopy, Dr. Irvine’s team observed the interaction between a single live staphylococcus bacterium and the surface of the stratum corneum and corneocytes. The team found that staphylococcus adheres strongly to these surfaces, particularly in patients with filaggrin (FLG) mutations. This bacterium is difficult to eliminate with topical or systemic antibiotics. It produces alpha toxins, which can destroy tight junctions and proteases that penetrate the stratum corneum. These findings highlight the extraordinary adaptability of S. aureus to the skin and its significant role in skin biology and impact on homeostasis.
3. S. aureus and Inflammation
The super antigen theory, which has been in existence for approximately 20 years, suggests that proteins such as protein A, a surface protein involved in the interactions with the immune response, interact with specific modules and directly instigate inflammation. S. aureus thrives on inflamed skin, penetrating deeply through the stratum corneum into the epidermis and dermis, where it becomes nearly impossible to eliminate. Some of these processes are facilitated through the TNF receptor. The activities of S. aureus are amplified in the presence of FLG-deficient epidermis and are further enhanced by type 2 cytokines. The type 2 immune response is designed to be a temporary defense mechanism against parasites, not against a constant inflammatory state over decades. When persistently activated, it directly compromises the skin barrier.
On a final note, on the microbiome, Elizabeth Grice’s team at the University of Pennsylvania examined commensals, the healthy microbiome. The discovery was made that these commensals operate via the AHR receptor to preserve the skin barrier. This is analogous to the way pollutants can worsen conditions if they induce a U-shaped curve. This underscores the importance of our normal microbiome in maintaining the skin barrier and mitigating inflammation.
Want to learn more about skin barrier dysfunction in AD? Follow the link to access the full webinar.
About the Author
Alan D. Irvine, MD, DSc
A key leader in dermatology research, he is a professor of Dermatology at Trinity College in Ireland. Dr. Irvine is the founding president of the Irish Skin Foundation. His research focuses on molecular genetics of skin disease including rare skin disorders.
Let’s shape the future of research and make a difference in the industry, gain Innovaderm’s support in your upcoming trial and propel your study to new heights.
To continue the conversation on dermatology clinical trials, do not miss out on our podcast: Phase Forward. Follow the link to subscribe now.
Newsletter
Newsletter subscription resources

